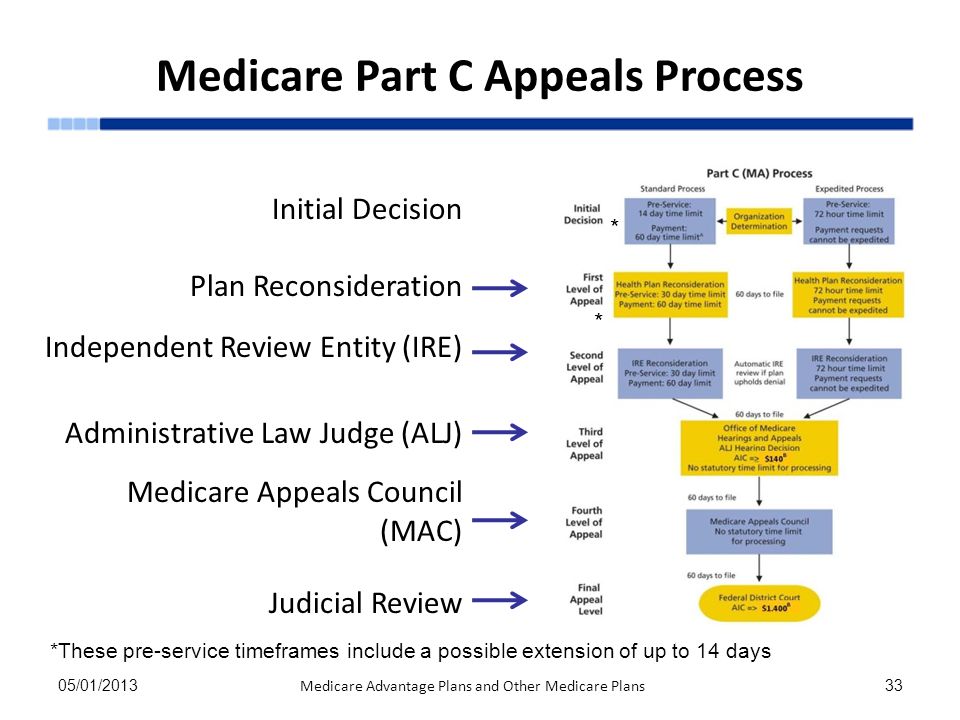
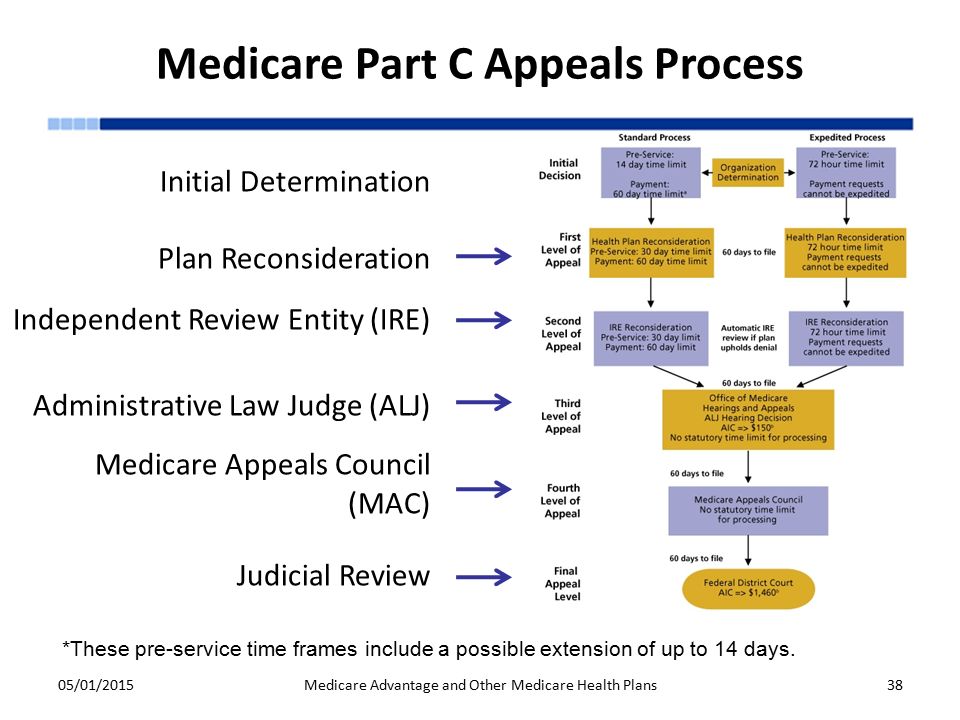
41 medicare appeals process diagram
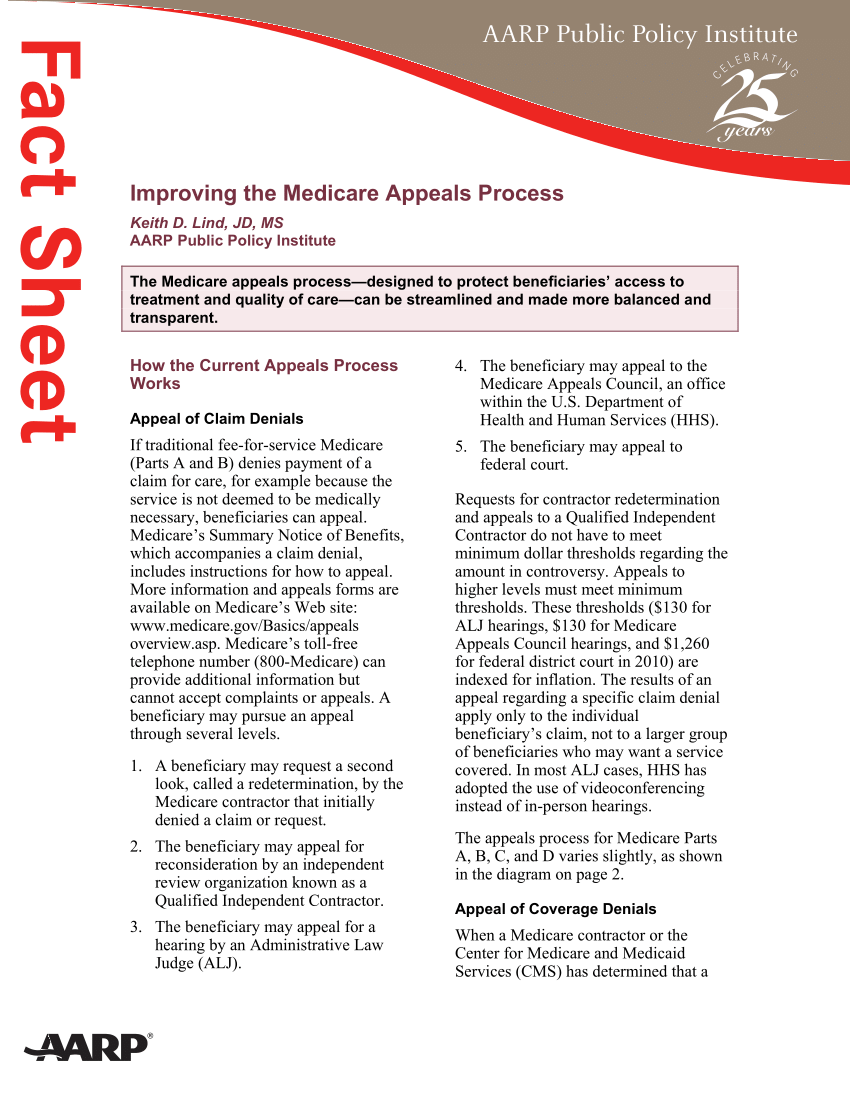
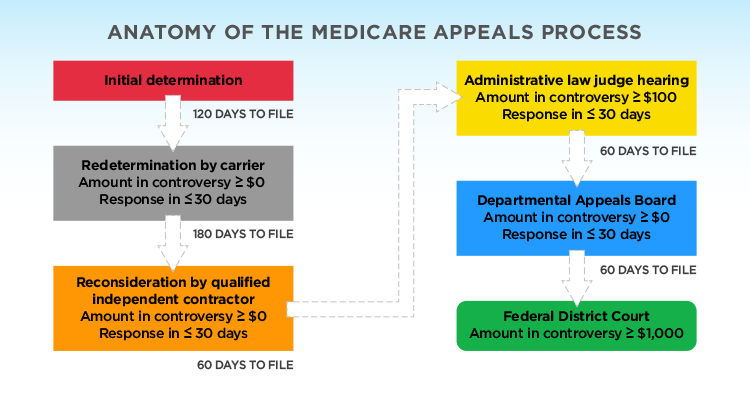
The 5 Levels of the Appeals Process. There are 5 levels of appeals available to you: Redetermination. Reconsideration. Administrative Law Judge (ALJ) Departmental Appeals Board (DAB) Review. Federal Court (Judicial) Review. Level 1 is a Redetermination, which is conducted by the DME MAC. A Redetermination is a completely new, critical re ... Augment your compliance and risk management teams with seasoned Medicare Advantage program policy experts, statisticians, physicians, data scientists and actuaries that provide expert medical record evaluation and reviews prior to or during the Medicare reconsideration and appeals process.
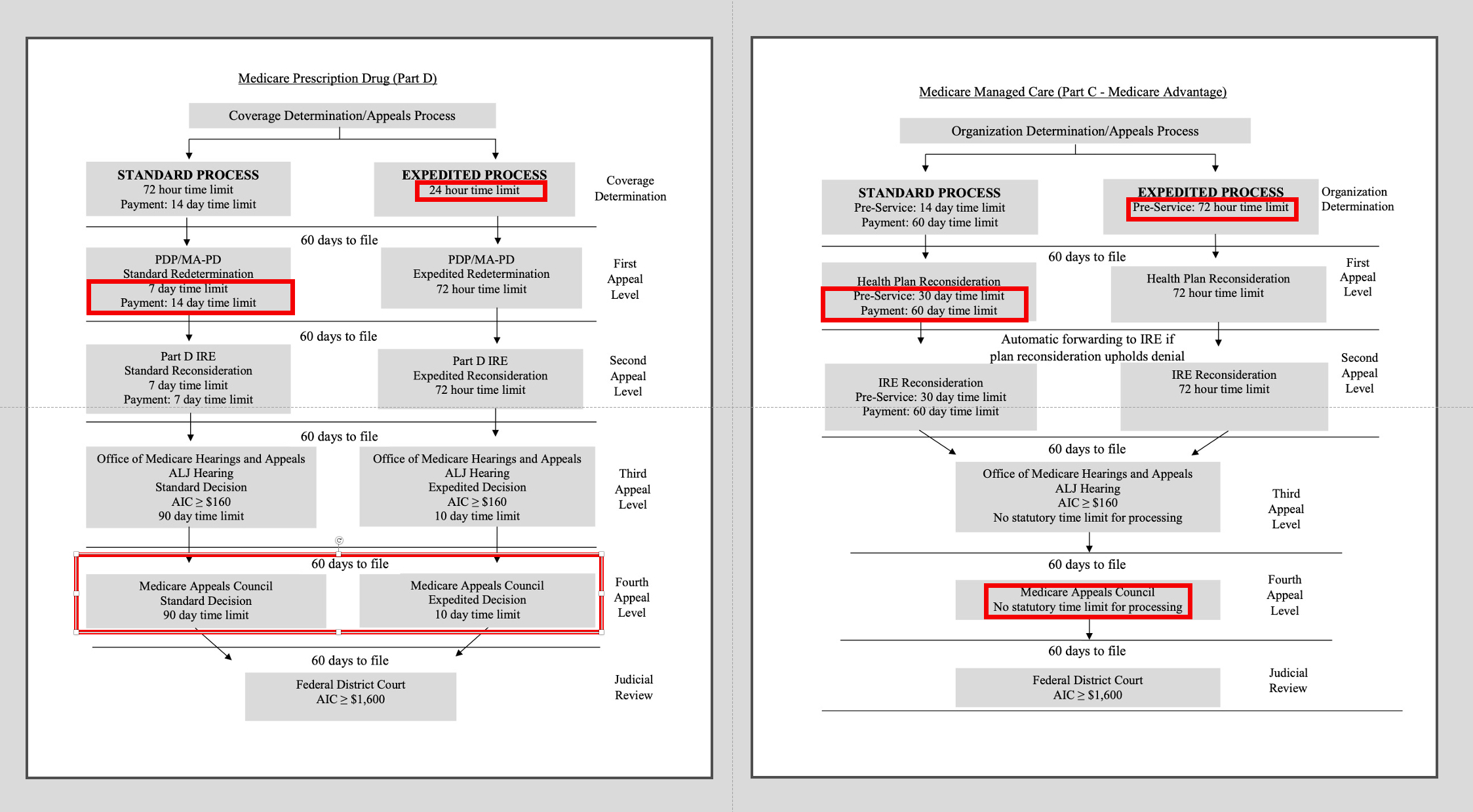
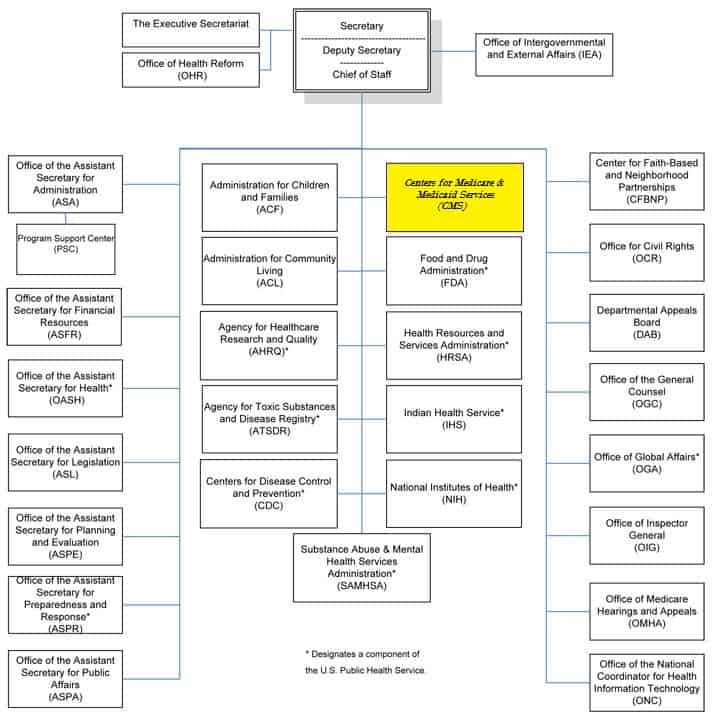
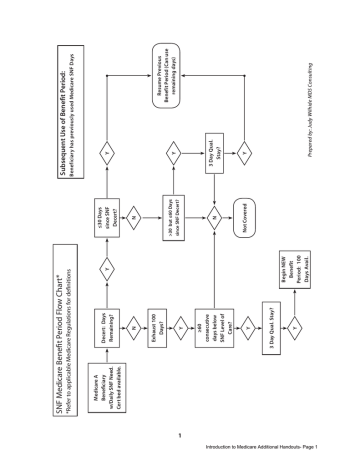
OMHA is responsible for Level 3 claims appeals. The entry point of the appeals process depends on the part of the Medicare program that covers the disputed benefit or whether the beneficiary is enrolled in a Medicare Advantage plan. There are five levels in the Medicare claims appeal process: Level 1: Your Health Plan. If you disagree with a Medicare coverage decision, you may request your health plan to redetermine your claim.
Medicare appeals process diagram
Your Level 1 appeal ("reconsideration") will automatically be forwarded to Level 2 of the appeals process in the following instances: Your plan does not meet the response deadline. If your Medicare Advantage plan fails to meet the established deadlines, it is required to forward your appeal to an independent outside entity for a Level 2 review. To see a diagram (flowchart) of the original Medicare (fee-for-service) standard and expedited appeals process, go to the "Downloads" section below. Appointment of Representative A party may appoint any individual, including an attorney, to act as his or her representative during the processing of a claim(s) and /or any claim appeals. Medicare Hearin gs and A ppeals ALJ Hearing AIC ≥ $180** No statutory time limit for processing . Medicare Appeals Council . No statutory time limit for processing . F. ederal District Court AIC ≥ $ Review1,760** First Appeal . Level Second Appeal Level Third Appeal Level Fourth Appeal Level Judicial
Medicare appeals process diagram. Conduct Claim Appeal Process Sequence Diagram: Table of Interface and Functional Descriptions ... Propose how the system assists the Billing Staff to automate and track the appeals process. ... It is desirable for a visual cue to be available to identify claims and their payment status. For Medicare and large events billing contains information ... What’s the appeals process for Original Medicare? The appeals process has 5 levels: Level 1: Redetermination by the Medicare Administrative Contractor (MAC) Level 2: Reconsideration by a Qualified Independent Contractor (QIC) Level 3: Decision by the Office of Medicare Hearings and Appeals (OMHA) Level 4: Review by the Medicare Appeals Council (Appeals Council) Medicare health plans, which include Medicare Advantage (MA) plans – such as Health Maintenance Organizations, Preferred Provider Organizations, Medical Savings Account plans and Private Fee-For-Service plans – Cost Plans and Health Care Prepayment Plans, must meet the requirements for grievance and appeals processing under Subpart M of the Medicare Advantage regulations. Reopenings are separate from the appeals process, and therefore, do not count towards the five levels of appeal. Note: Reopenings (TOB XXQ) cannot be submitted with a hardcopy (paper) UB-04. They must be submitted via the 5010 format or entered directly into the Fiscal Intermediary Standard System (FISS) via Direct Data Entry (DDE).
8581.1 Medicare Contractors shall accept new bill type frequency code “Q” for all institutional claim bill types and adjust any shared system reason codes as necessary. X X X X COBA, HIGLAS 8581.2 Medicare Contractors shall accept and develop edits that require a condition code in the R1-R9 series if the Settled appeals are dismissed Step 10 CMS sends fully executed agreement and Settlement Step 11 Yes Process Over CMS, Appellant & MAC develop consensus Spreadsheet Step 5 Is consensus reached? No Yes Process Complete Low Volume Appeal Settlements Appellant Process Diagram Within 30 days Within 15 days Within 180 days Within 30 days Within 15 ... Joint Capabilities Integration and Development System (JCIDS) Process Flow Chart - Rev 1.0 for JCIDS Manual dated 19 Jan 2012. JC. S. O. READ MORE on www.acqnotes.com. Chapter 1. Introduction - SL1 Documentation - ScienceLogic. Download this manual as a PDF file. In the image above, the steps display as part of the flowchart in the main ... Claim denials from Medicare, Medicaid and health plans are on the rise, and understanding recent trends in denials is essential to the development of an effective and comprehensive appeal strategy. Among those emerging trends, distinguishing coding denials from clinical validation denials (CVDs) is an ongoing challenge.
The Medicare Advantage plan has information about how to start the appeal process. If you feel you may get worse by waiting too long, you can ask for an expedited appeal. This means the Medicare Advantage plan must make a decision about the appeal within three calendar days. If you need this faster review, ask your Medicare Advantage plan for ... 1. Complaints Process, two-page document 2. Medicare Appeals, 60 -page booklet 3. Making Sense of Your Medicare Statements, three-page document 4. Medicare redetermination reque st form — 1st Level of appeal, one- page document 5. Welcome to Livanta, the BFCC-QIO for Washington, one- page document 6. Which of the following are the steps to finding the correct ICD-10-CM code? (Select the three (3) correct answers.) Identify the main term., Look up the main term in the Alphabetic Index., Note all essential modifiers. A patient presents with her two insurance ID cards, Medicare and BCBS. She turned 65 six months ago, but plans to continue ... The provider can then follow a formal appeals process specific to each payer. This can be a protracted, multi-step process that requires a material amount of time from providers and insurers alike. Level One: The initial phase begins with the doctor and patient contacting the payer to demonstrate that the requested treatment is medically ...
The process for coverage decisions and making appeals deals with problems related to your benefits and coverage for a medical item/service and Part B prescription drugs, including problems related to payment. This is the process you use for issues such as whether something is covered or not and the way in which something is covered.
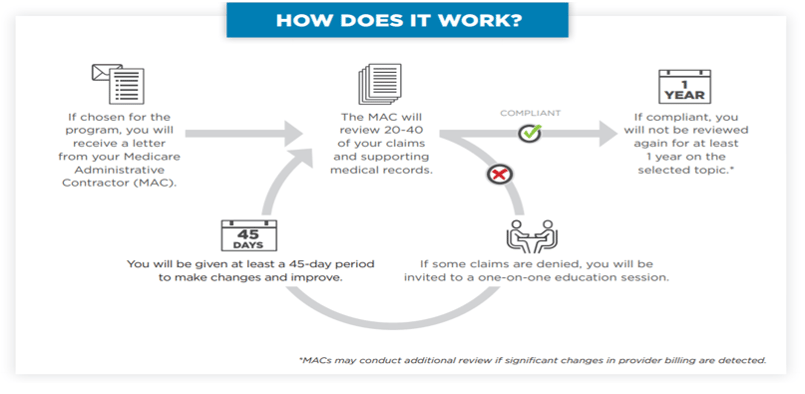
The Medicare Administrative Contractor (MAC) may initiate claim adjustments and/or overpayment recoupment actions through the standard recovery process. Questions. If you have questions about the overpayment recovery process or appeal rights, find and contact your MAC using the review contractor directory.
Using Matched Survey And Administrative Data To Estimate Eligibility For The Medicare Part D Low Income Subsidy Program
Apache Server at www.seniorcitizensguide.com Port 80
program, Medicare. Medicare is a health insurance program primarily for elderly persons, regardless of income. It is financed through Social Security taxes and premiums. Medicaid is jointly financed by the state and federal governments and is designed to provide health care to low income individuals. Medicaid started in
If you disagree with your plan's initial decision, you can file an appeal. The appeals process has 5 levels. If you disagree with the decision made at any level of the process, you can generally go to the next level. At each level, you'll get instructions in the decision letter on how to move to the next level of appeal.
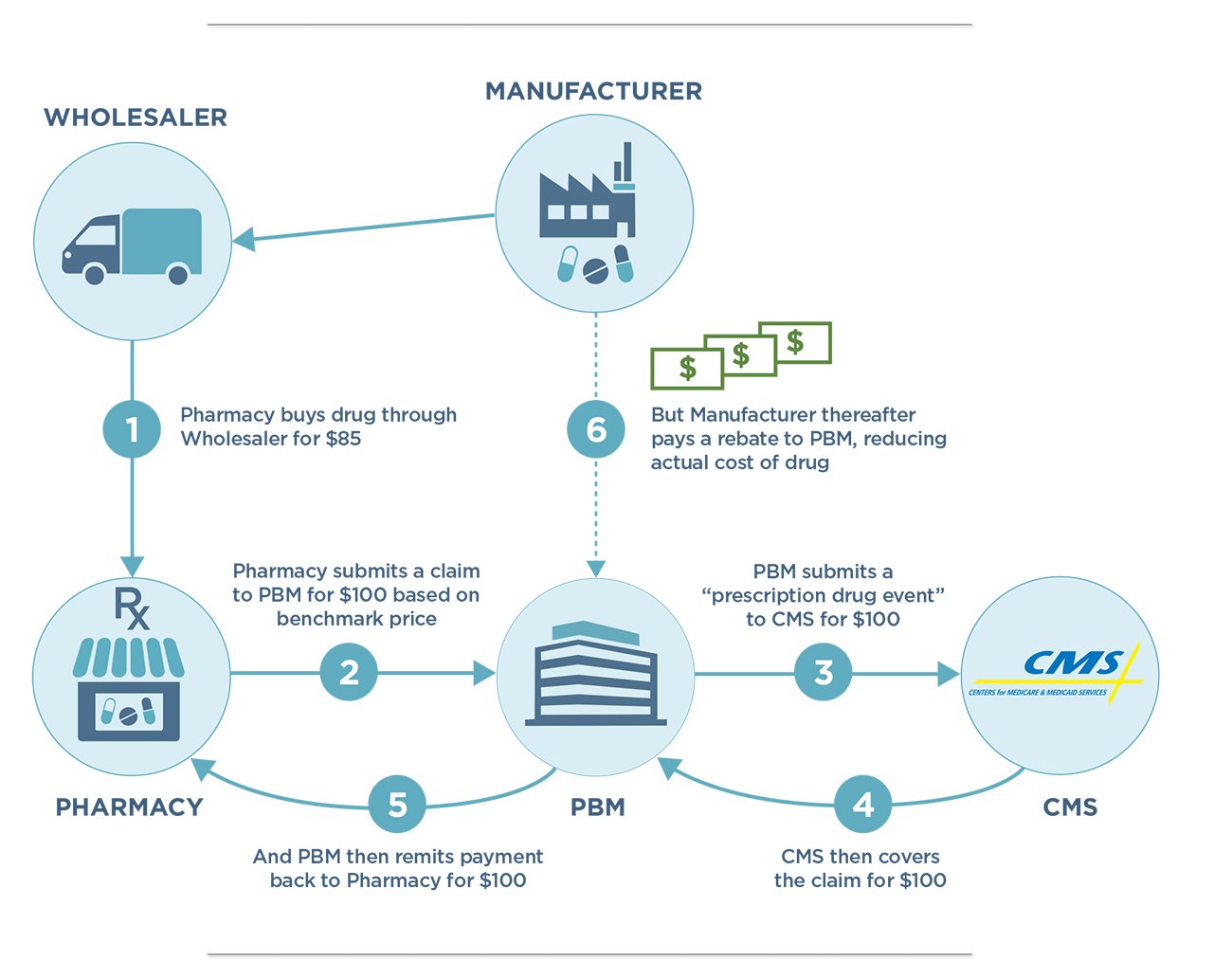
Pbm Dir Fees Costing Medicare And Beneficiaries Investigate White Paper On Background Cost Impact And Legal Issues Community Oncology Alliance
Medicare Appeals Process: There are 5 steps after an initial denial (coverage determination)from the insurance company that may take place to substantiate a patients or providers request for a particular non covered medication. 1. Level 1: Redetermination from plan (Appeal)-can be for any denied coverage
5 things to know when filing an appeal. If you decide to file an appeal, ask your doctor, health care provider, or supplier for any information that may help your case. If you think your health could be seriously harmed by waiting for a decision about a service, ask the plan for a fast decision. If the plan or doctor agrees, the plan must make ...
File an appeal. How to appeal a coverage or payment decision made by Medicare, your health plan, drug plan or Medicare Medical Savings Account (MSA) Plan. Your right to a fast appeal. Learn how to get a fast appeal for Medicare-covered services you get that are about to stop. Your Medicare rights. Understand your Medicare options, rights, and ...
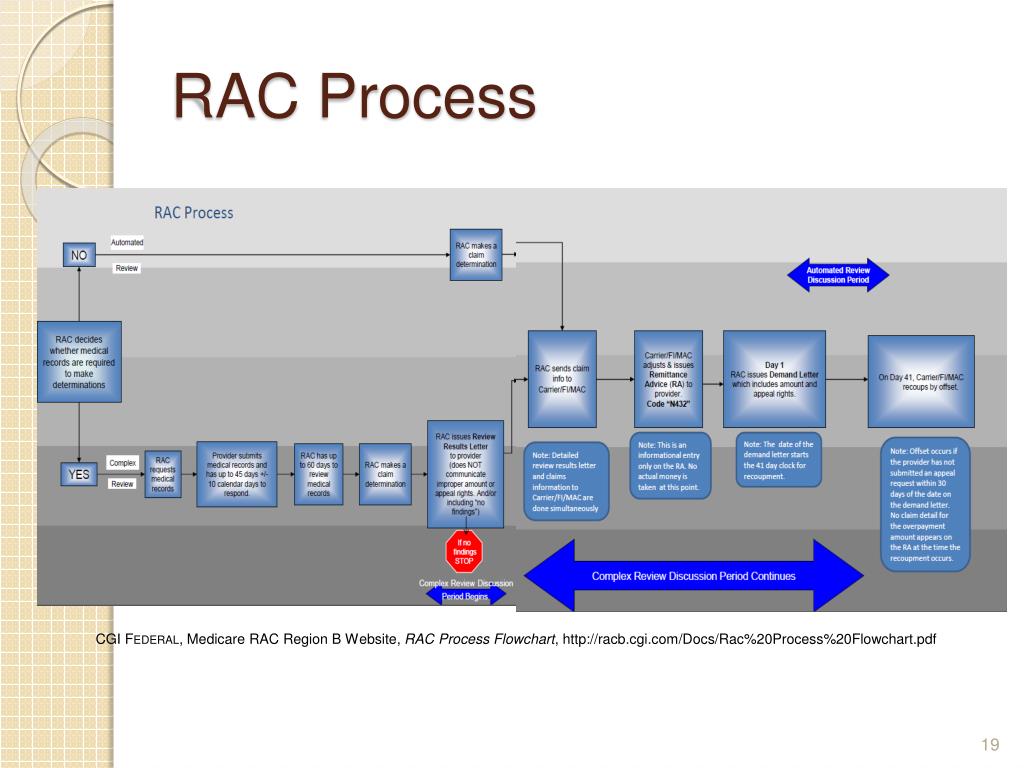
Ppt Midwest Home Health Summit Best Practices Conference Series Medicare And Medicaid Audit Defense Appeals From R Powerpoint Presentation Id 1406155
Which of the following are the basic steps of the general appeal process? (Select all that apply.) Appeal Complaint Grievance. List the five steps of the Medicare appeal process in correct order, starting with the first one at the top. 1. Redetermination 2. ... Diagrams. Flashcards. Mobile. Help. Sign up. Help Center. Honor Code. Community ...
List and describe the steps involved in the Medicare appeals process. Step 4, MAC review request must be filed within 60 days f receipt of the ALJ's decisions. If council does not issue a decision on a provider-initiated review within 90 days, provider may request escalation to the next step, which is filing with federal district court.
Qualified Independent Contractors (QICs) that process 2nd level Medicare. QIC Appeals Portal at qicappeals.cms.gov, or by fax to 585-869-3346. appeal reconsiderations, is through your Medicare Administrative Contractor ( MAC) portal. To see a diagram (flowchart) of the original Medicare (fee-for- service).
Appendix C to Part 92—Sample Section 1557 of the Affordable Care Act Grievance Procedure. It is the policy of [Name of Covered Entity] not to discriminate on the basis of race, color, national origin, sex (including pregnancy, sexual orientation, and gender identity), age or disability.[Name of Covered Entity] has adopted an internal grievance procedure providing for prompt and equitable ...
If you have a Medicare health plan, start the appeal process through your plan. Follow the directions in the plan's initial denial notice and plan materials. You, your representative, or your doctor must ask for an appeal from your plan within 60 days from the date of the coverage determination.
The first step in the Medicare appeals process is _____ redetermination If a Medicare beneficiary receives treatment by workers compensation, the Medicare plan is __________
How to file an appeal if your Medicare Advantage Plan doesn't cover an item or service If you have a Medicare Advantage Plan, you know it covers a lot of items and services, like prescription drugs, diabetic test supplies, cardiovascular screenings, and hospital visits.
- An appeal process is used to challenge a payer's decision to deny, reduce, or otherwise downcode a claim - Each payer has a graduated level of appeals, deadlines for requesting them, and medical review programs to answer them - In some cases, appeals may be taken beyond the payer to an outside authority, such as a state insurance commission
Medicare Plus Blue PPO Provider Manual Page vi Medicare Plus Blue PPO Provider Manual Revised January 2020. MA PPO . Prior authorization of skilled nursing facility, long-term acute care, and inpatient rehabilitation
appeals process to their services. Find more information on the . CMS Appeals and Medicare Appeals webpages. Appealing Medicare Decisions Medicare FFS has 5 appeal process levels: Level 1 - MAC. Redetermination. Level 2 - Qualified Independent Contractor (QIC) Reconsideration. Level 3 - Office of Medicare Hearings and Appeals (OMHA) Disposition. Level 4 -
Medicare Hearin gs and A ppeals ALJ Hearing AIC ≥ $180** No statutory time limit for processing . Medicare Appeals Council . No statutory time limit for processing . F. ederal District Court AIC ≥ $ Review1,760** First Appeal . Level Second Appeal Level Third Appeal Level Fourth Appeal Level Judicial
To see a diagram (flowchart) of the original Medicare (fee-for-service) standard and expedited appeals process, go to the "Downloads" section below. Appointment of Representative A party may appoint any individual, including an attorney, to act as his or her representative during the processing of a claim(s) and /or any claim appeals.
Your Level 1 appeal ("reconsideration") will automatically be forwarded to Level 2 of the appeals process in the following instances: Your plan does not meet the response deadline. If your Medicare Advantage plan fails to meet the established deadlines, it is required to forward your appeal to an independent outside entity for a Level 2 review.

Examining The Prior Authorization Process Patient Outcomes And The Impact Of A Pharmacy Intervention A Single Center Review Journal Of The American Academy Of Dermatology

The Insurance Approval Process For Proton Radiation Therapy A Significant Barrier To Patient Care International Journal Of Radiation Oncology Biology Physics















0 Response to "41 medicare appeals process diagram"
Post a Comment